post
Common Myths About ADHD Diagnosis
Common Myths About ADHD Diagnosis: Debunking Misconceptions
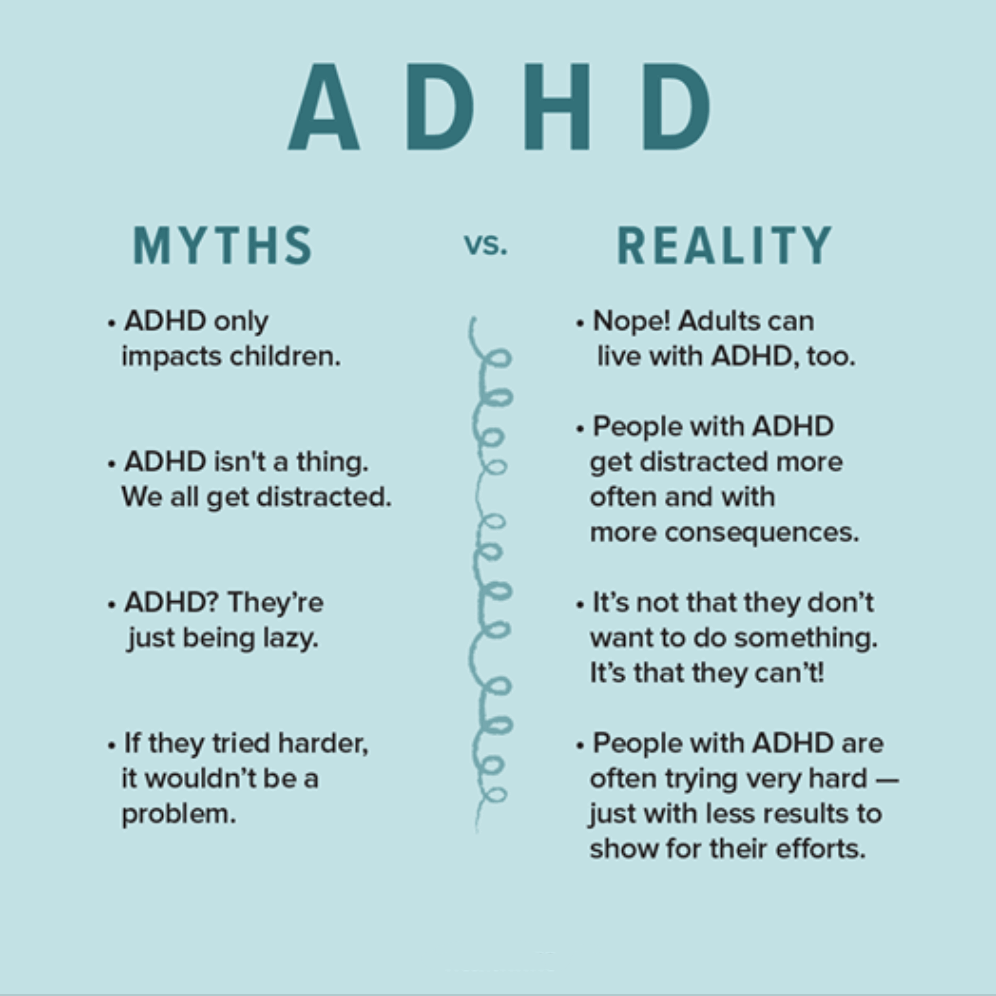
The conversation around Attention-Deficit/Hyperactivity Disorder (ADHD) has grown significantly in recent years, leading to increased awareness. However, this surge in information has also brought a rise in misconceptions, particularly regarding the diagnosis process. These common myths about ADHD diagnosis can create significant barriers, causing individuals and families to delay seeking help, doubt a professional’s findings, or dismiss the reality of the condition altogether.
An accurate diagnosis is the crucial first step toward understanding and effectively managing ADHD. It’s not a label, but a roadmap for tailored support, therapy, and, if appropriate, medication. This comprehensive guide will systematically debunk the most prevalent myths surrounding the ADHD diagnostic process, clarify the actual assessment steps, and underscore the vital importance of receiving a professional, accurate diagnosis.
Myth 1: “ADHD is Overdiagnosed and Everyone Has a Little Bit of It.”
This is perhaps the most pervasive and damaging of the common myths about ADHD diagnosis. The idea that every easily distracted person or energetic child is being labeled with ADHD diminishes the struggle of those who truly have the disorder.
The Reality of Diagnosis
- Prevalence: Studies consistently show that ADHD has a stable, biological prevalence rate, typically around 5-7% of children and 2.5-5% of adults globally. While awareness has increased, leading to more people being assessed, this doesn’t equate to overdiagnosis. It suggests we are getting better at identifying those who meet the strict diagnostic criteria.
- Strict Criteria: Diagnosis is not based on a single symptom. Clinicians use the detailed criteria set forth in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
- Symptoms of inattention (e.g., poor attention to detail, difficulty organizing tasks, losing things) and/or hyperactivity-impulsivity (e.g., fidgeting, interrupting others, feeling restless) must be present.
- A specific number of symptoms must be met (e.g., six or more for children; five or more for adults).
- Symptoms must be present before the age of 12.
- Symptoms must persist for at least six months.
- Symptoms must occur in two or more settings (e.g., home, school, work, social activities).
- There must be clear evidence that the symptoms interfere with, or reduce the quality of, social, academic, or occupational functioning.
A professional diagnosis is a rigorous process, not a casual one. It’s an evaluation that requires significant impairment, distinguishing it from normal levels of distractibility or energy.
Myth 2: “Adults Can’t Be Diagnosed with ADHD Because You Only Get It as a Kid.”
This is one of the biggest reasons adults suffer for years without treatment, believing they are simply lazy, disorganized, or flawed. They assume if they didn’t have a diagnosis as a child, they can’t have it now.
ADHD is a Lifespan Condition
ADHD is a neurodevelopmental disorder, meaning it starts in childhood. The DSM-5 criteria explicitly require that several symptoms were present before the age of 12. However, this does not mean an official diagnosis must have occurred in childhood.
- Late Identification: Many adults slip through the cracks because:
- They were gifted/high-IQ and were able to compensate academically until their college or career workload became overwhelming.
- They had the inattentive presentation (formerly known as ADD), where symptoms like daydreaming and disorganization were overlooked because they didn’t cause disruptive classroom behavior.
- Their symptoms were misattributed to anxiety, depression, or a personality flaw.
- The Adult Diagnostic Process: A skilled clinician diagnosing an adult will:
- Take a thorough developmental history, often involving talking to parents or reviewing old report cards to confirm the childhood onset of symptoms.
- Use standardized adult rating scales (like the ASRS or Conners’ Adult ADHD Rating Scales).
- Assess the current impact on work, relationships, and home life.
A new diagnosis in adulthood simply means the condition was identified later, not that it began later.
Myth 3: “The Doctor Just Diagnosed It After a 15-Minute Chat and Giving a Prescription.”
The idea that ADHD is diagnosed after a quick, superficial conversation feeds the “overdiagnosis” myth and undermines faith in legitimate clinicians. While some unethical practitioners may exist, a proper ADHD evaluation is comprehensive and multi-faceted.
A Thorough Evaluation Includes:
- Clinical Interview (1-3 hours): A deep discussion with the individual (and often a parent/partner for collateral information) covering:
- Current symptoms and their impact.
- Developmental history, including academic and behavioral reports from childhood.
- Family medical history (ADHD is highly heritable).
- Social, educational, and occupational functioning.
- Standardized Rating Scales: The individual and often one or more observers (parent, teacher, partner) complete standardized, validated questionnaires (e.g., Vanderbilt, Conners’, ADHD Rating Scale-5) that measure symptom frequency and severity relative to age/gender norms.
- Differential Diagnosis: This is arguably the most critical step. The clinician must rule out other conditions that can mimic ADHD symptoms, such as:
- Anxiety disorders.
- Major depressive disorder.
- Thyroid issues or sleep disorders.
- Side effects of medication.
- Post-traumatic stress disorder (PTSD).
- Neuropsychological Testing (Optional but Comprehensive): In complex cases, a comprehensive battery of tests may be administered to assess cognitive functions like working memory, processing speed, and sustained attention. While no single cognitive test can diagnose ADHD, they provide objective data on cognitive deficits often associated with the disorder.
- Review of Documents: Old report cards, disciplinary notices, and previous medical records are often reviewed for historical evidence of impairment.
A diagnosis based solely on a 15-minute checklist or an immediate prescription is a significant red flag. A proper assessment takes time, data from multiple sources, and the clinical expertise to differentiate ADHD from other conditions.
Myth 4: “ADHD is a Diagnosis Based Only on Subjective Checklists, Not Objective Brain Scans.”
Many people mistakenly believe that without a definitive blood test or brain scan, the diagnosis is fundamentally unreliable. They often ask, “Can’t you just give me a brain test for it?”
Why Objective Tests Are Limited (For Now)
It is true that ADHD diagnosis relies on a clinician’s judgment based on behavioral criteria. However, this is similar to the diagnosis of many other mental health conditions, like anxiety or autism, which are also based on observed symptoms and functional impairment.
- No Single “ADHD Gene” or “ADHD Brain Scan”: While research has identified structural and functional differences in the brains of people with ADHD—particularly in the prefrontal cortex related to executive functions—these findings are based on group averages and are not specific enough to diagnose an individual.
- QEEG and Computerized Tests: Some clinics offer quantitative electroencephalography (QEEG) or computerized performance tests (like the Continuous Performance Test – CPT). These tools can provide objective data on attention performance and brain activity patterns.
- Value: They can support a clinical impression, track treatment efficacy, and help rule out some other issues.
- Limitation: They cannot diagnose ADHD alone. A person can perform poorly on a CPT due to boredom, anxiety, or lack of sleep, not necessarily ADHD. The DSM-5 criteria remain the gold standard.
An experienced clinician uses behavioral reporting, historical context, and the elimination of other causes (differential diagnosis) to make a reliable diagnosis—a process that is far from purely subjective.
Myth 5: “ADHD Diagnosis is Only for Hyperactive Boys Who Disrupt Class.”
This myth often leads to the underdiagnosis of two major groups: girls/women and individuals with the Predominantly Inattentive Presentation (ADHD-PI).
The Diverse Faces of ADHD
- The Gender Gap: ADHD in girls often presents differently than the stereotypical hyperactive boy. Girls are more likely to exhibit:
- The Predominantly Inattentive Presentation.
- Internalizing behaviors like anxiety, low self-esteem, and social withdrawal.
- Verbal hyperactivity (excessive talking) rather than physical hyperactivity.
- Perfectionism and chronic attempts to overcompensate for organizational difficulties.
- Clinicians unfamiliar with these subtle presentations may overlook their symptoms entirely.
- The Inattentive Presentation: This presentation, characterized by symptoms like disorganization, forgetfulness, difficulty sustaining focus, and “losing track” during conversations, often goes undiagnosed for years.
- Common Mislabels: Individuals are frequently labeled as spacey, lazy, unmotivated, or simply having learning disabilities.
- Impact: Without the disruptive behavior of hyperactivity, the inattentive type doesn’t draw the same attention from teachers or parents, delaying intervention.
An accurate diagnosis requires the clinician to recognize that ADHD has three distinct presentations: Combined, Predominantly Inattentive, and Predominantly Hyperactive/Impulsive.
Myth 6: “If You Can Focus on Video Games or Hobbies, You Don’t Have ADHD.”
This is perhaps the most confusing point for patients and a common self-doubt barrier. People with ADHD often experience hyperfocus—an intense, sometimes obsessive ability to concentrate on tasks they find stimulating or intrinsically rewarding.
The Role of Interest and Stimulation
The defining feature of ADHD is not an inability to focus, but rather an inconsistency of attention driven by the brain’s dopamine and executive function systems.
- Executive Function Deficits: ADHD is a disorder of attention regulation, not attention capacity. The ability to focus on a boring but necessary task (like paperwork) is impaired, while the ability to focus on a high-interest, high-stimulation task (like video games or a creative project) remains intact or is even heightened (hyperfocus).
- Reward Circuitry: Tasks that provide immediate, novel, or intense gratification (high dopamine release) can bypass the need for typical executive control.
- Diagnostic Relevance: A clinician will specifically ask how attention is inconsistent—does the person struggle with homework, chores, or work reports, but succeed at hobbies? If the person can only sustain focus on stimulating tasks, and struggles with all others, this supports the diagnosis, rather than refuting it.
The capacity for hyperfocus is a hallmark of the ADHD brain, not an exclusion criterion.
- ADHD DRUGS8 products
- ANXIETY AND DEPRESSION6 products
- BEST SELLING PILLS12 products
- OPIOIDS DRUGS4 products
- PAIN RELIEF DRUGS17 products
The Importance of Accurate Diagnosis: Why Debunking Myths Matters
Debunking these common myths about ADHD diagnosis is more than just correcting information—it is critical to ensuring people get the help they need. An accurate diagnosis provides:
- Validation: For many, realizing their lifelong struggles are due to a neurobiological difference, not a personal or moral failure, is immensely relieving. It transforms the question from “What is wrong with me?” to “How does my brain work?“
- Targeted Treatment: An accurate diagnosis allows for the creation of a personalized treatment plan, which may include:
- Psychoeducation: Understanding how the condition affects the individual.
- Behavioral Therapy: Learning coping skills, time management, and organizational strategies.
- Medication: For many, stimulant or non-stimulant medication can significantly improve focus and reduce impulsivity, making therapy and daily functioning more effective.
- Accommodation: Diagnosis provides access to formal accommodations in educational settings (IEPs/504 Plans) and workplaces (ADA/Disability Services), ensuring fair opportunities.
- Co-occurring Conditions: The diagnostic process often uncovers or clarifies co-occurring conditions (e.g., anxiety, depression, learning disorders) which are common in individuals with ADHD, allowing for holistic treatment.
By understanding the realities of the diagnostic process its thoroughness, the strict criteria, and the expertise required for differential diagnosis we can move past the harmful myths and focus on empowerment and support for those with ADHD. If you or a loved one suspects ADHD, seeking an evaluation from a qualified mental health professional (psychologist, psychiatrist, or neurologist) specializing in adult or child ADHD is the most important step forward.
